Home > about eyes > Keratoconus
Keratoconus
What is Keratoconus
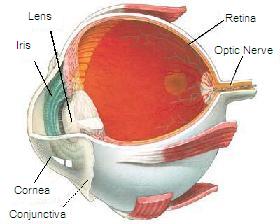 |
The cornea is the window of the eye. Light travels through the cornea past the lens to the retina and then the brain to form a visual image. The normal corneal surface is smooth and aspheric i.e. round in the center, flattening towards its outer edges. Light rays passing through it moves in an undistorted manner to the retina to project a clear image to the brain. In patients with keratoconus the cornea is cone shaped (hence the name keratoconus, derived from the greek word for cornea (‘kerato’) and cone shaped (‘conus’). In patients with keratoconus the cornea is not only cone shaped but the surface is also irregular resulting in a distorted image being projected onto the brain. |
Because the cornea is irregular and cone shaped, glasses do not adequately correct the vision in patients with keratoconus since they cannot conform to the shape of the eye. Patients with keratoconus see best with rigid contact lenses since these lenses provide a clear surface in front of the cornea allowing the light rays to be projected clearly to the retina. Hence the vast majority of patients are treated with rigid contact lenses. There are however some excellent new surgical options for patients with keratoconus who cannot tolerate these lenses, these options are discussed under treatments for keratoconus.
DetectionMany patients are initially unaware they have keratoconus and see their eye doctor because of increasing spectacle blur or progressive changes in their prescription. In many instances even a good refraction yields poor vision. Keratoconus is most often diagnosed by a cornea specialist who may see typical findings when examining the patient at the slit-lamp. In early forms of the disease there may be no obvious finding on slit-lamp evaluation and the diagnosis is made by computerized videokeratography only. |
 |
Occurrence
Keratoconus typically commences at puberty and progresses to the mid thirties at which time progression slows and often stops. Between age 12 and 35 it can arrest or progress at any time and there is no way to predict how fast it will progress or if it will progress at all. In general young patients with advanced disease are more likely to progress to the point where they may ultimately require some form of surgical intervention.
Keratoconus may occur in one eye only initially but most commonly affects both eyes with one eye being more severely affected than the other. Both males and females are equally affected and there is no ethnic predilection though in some parts of the world including New Zealand and in certain parts of Finland there is a higher incidence due to genetic factors.
Causes
Despite millions of dollars being spent on keratoconus no one truly knows the cause of the disease. There have been many interesting theories but none of them have yet been proven conclusively neither have any of them consistently been reproduced by multiple research groups. One theory suggests eye rubbing causes the progression of keratoconus. The evidence for this is however anecdotal based on several case reports, but there is no reproducible scientific evidence to support it. Others suggest that there is deficient collagen crosslinking caused by free radicals, interesting progress has been made in this area (see below).
For further information please contact our clinic
Treatments
| New Zealand (North Island) residents with keratoconus may be eligible for a Ministry of Health subsidy towards the fitting and supply of contact lenses. The subsidy is managed between the optometrist and the MOH, please contact us for further information. |
 |
Cornea Cross Linking Treatment (C3R)
In New Zealand, a country with a high prevalence of keratoconus and the highest reported rate of corneal transplant surgery for keratoconus in the world, collagen cross-linking has the potential to become a very important sight-preserving treatment. The C3R process, using riboflavin (a B-complex vitamin) solution combined with UVA exposure, was developed in Germany from 1993 onwards with the first patients treated in 1998. (1)
Because it is less invasive than corneal transplant, the patient's surgery-related risks are reduced. As a less expensive, technically simpler procedure, collagen crosslinking could be particularly useful in developing countries where corneal transplant and other procedures may be difficult to access.
In some cases, crosslinking may also be successfully combined with other treatment methods such as corneal ring segment inserts (2). Corrective lenses may still be required after these treatments but with more normal prescriptions possible now, and these newer methods may have an important role in limiting deterioration of vision, increasing unaided/uncorrected vision and reducing the case for corneal transplantation. (1)
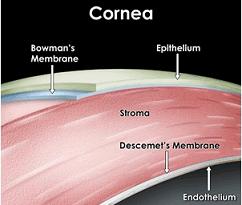 |
Collagen is the primary protein constituent of the body's connective tissues. The riboflavin causes new bonds to form across adjacent collagen strands in the stromal layer of the cornea, which recovers and preserves some of the cornea's mechanical strength. The corneal epithelial layer is generally removed in order to increase penetration of the riboflavin into the stroma. (Wikipedia) The procedure helps restore appropriate curvature and structure to the cornea, and makes it possible for most patients who need them to wear rigid contact lenses again.(2) |
In some cases, crosslinking may also be successfully combined with other treatment methods such as corneal ring segment inserts (2). Corrective lenses may still be required after these treatments but with more normal prescriptions possible now, and these newer methods may have an important role in limiting deterioration of vision, increasing unaided/uncorrected vision and reducing the case for corneal transplantation. (1)
INTACS
| A method for flattening the cornea that is too steep and making a patient more contact lens tolerant is the insertion of INTACS into the cornea. This procedure is good for patients who are contact lens intolerant and who want to avoid a corneal transplant and whose K readings are not in excess of 58 Diopters. It is also useful for individuals with keratoconus who want to improve their present vision with or without contact lenses. This technique involves the insertion of two arc like plastic segments into the middle of the cornea to flatten the cornea. This procedure was pioneered 8 years ago in France, and is routinely being done by many cornea specialists in the New Zealand. |
 |
INTACS surgery is not truly reversible because of the incision, but the INTACS can be completely removed or exchanged for a different size. Inserts cannot be felt by the patient and are no more visible than a contact lens. After insertion and healing, they require no maintenance.
The placement of INTACS inserts remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus. Follow-up visits will be required to monitor the healing process and to evaluate the visual benefits of the procedure. Even after a successful Intacs procedure for keratoconus, glasses or contacts may be required, however Intacs have been shown to improve vision and reduce or stop the progression of keratoconus, thereby saving the patient from needing PKP.(3)
The placement of INTACS inserts remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus. Follow-up visits will be required to monitor the healing process and to evaluate the visual benefits of the procedure. Even after a successful Intacs procedure for keratoconus, glasses or contacts may be required, however Intacs have been shown to improve vision and reduce or stop the progression of keratoconus, thereby saving the patient from needing PKP.(3)
Contact Lenses
Patients with very mild disease may initially be corrected with glasses or soft contact lenses, however the vast majority of patients need rigid contact lenses for adequate vision correction.
Many patients find their contact lenses uncomfortable and can only tolerate them for a short period of time. One reason this happens is that the cornea steepens and rubs against the lens causing an abrasion and light sensitivity. Another reason is patients with keratoconus often have very dry eye and as the eye dries out there is no lubricating barrier between the lens and the cornea contributing to the patient being uncomfortable. There are now many ways to treat dry eyes to improve contact lens tolerance. This includes:
- the use of artificial tears,
- treating the lids for lid disease,
- Restasis– for increasing tear production and
- the use of punctal plugs to prevent tears from draining down your nasolacrimal ducts and keeping the eye moist.
Lens discomfort:
Sometimes a little scar or nebulous appears on the tip of the cornea that constantly rubs against the lens making it difficult to tolerate contact lenses, this scar can be removed with a blade or with the Excimer laser to return patients to contact lens tolerance – this procedure is called phototherapeutic keratectomy(PTK) or nebulectomy.
Please feel free to contact us for further information.
References
1. Dr Adam Watson, Auckland NZ, Published in New Zealand Optics Magazine April 2008
2. ScienceDaily (Nov. 9, 2008)
3. Br J Ophthalmol. 2010 Aug 1;
- 'Piggy-backing' contact lenses is used especially where keratoconus patients are particularly sensitive to hard lenses, yet require them. A soft contact lense is worn beneath the hard for added comfort and to build up tolerance.
- 'Synergize hybrid contact lens' are an option in some cases, they are rigid in the middle and soft on the edges and have the potential to give you the good quality vision of the rigid lens with some of the comforts of the soft lens.
Sometimes a little scar or nebulous appears on the tip of the cornea that constantly rubs against the lens making it difficult to tolerate contact lenses, this scar can be removed with a blade or with the Excimer laser to return patients to contact lens tolerance – this procedure is called phototherapeutic keratectomy(PTK) or nebulectomy.
Please feel free to contact us for further information.
References
1. Dr Adam Watson, Auckland NZ, Published in New Zealand Optics Magazine April 2008
2. ScienceDaily (Nov. 9, 2008)
3. Br J Ophthalmol. 2010 Aug 1;



